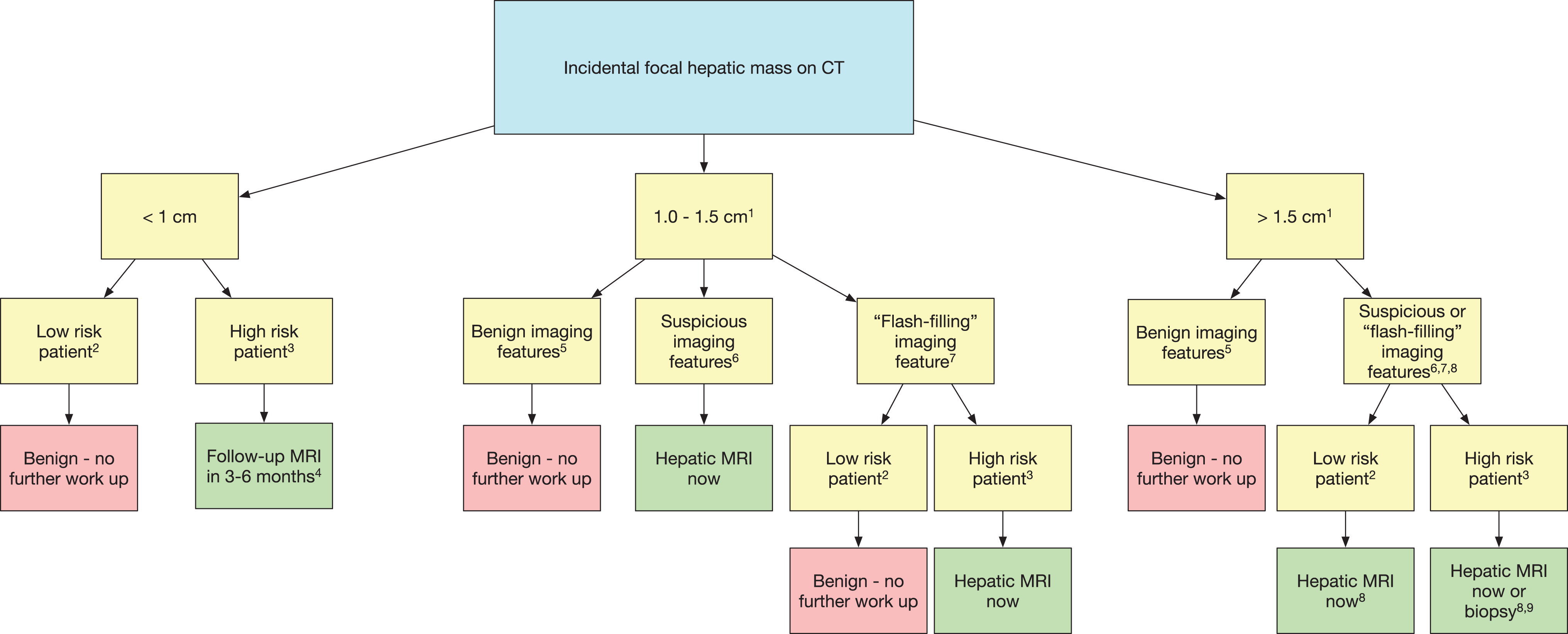
Incidental lesions on CT
1If inadequate imaging is available to ascertain the presence of benign versus malignant features in a > 1 cm mass, MRI is advised.
2Low-risk patient: no known primary malignancy or hepatic risk factors (cirrhosis, hepatitis, alcoholism, nonalcoholic steatohepatitis, sclerosing cholangitis, primary biliary cirrhosis, choledochal cyst, hemochromatosis and other hereditary hepatic conditions, anabolic steroid use, or elevated tumor markers).
3High-risk patient: history of malignancy or hepatic risk factors as previously defined.
4Follow-up MRI in 3 to 6 months. May need shorter term follow-up in some scenarios. Computed tomography follow-up is also acceptable in a patient with cancer who is due for routine CT surveillance.
5Benign features: sharp well-defined margin, homogeneous low attenuation (< 20 HU) and characteristic features of hemangiomas, FNH, focal fatty sparing or deposition, or perfusional changes. If pseudoenhancement is present, a benign cyst may measure > 20 HU; radiologist discretion is necessary.
6Suspicious features: ill-defined margins, heterogeneous density, mural thickening or nodularity, thick septa, and intermediate to high attenuation on portal venous phase imaging (> 20 HU in the absence of pseudoenhancement). If both pre- and postcontrast CT is available, enhancement > 20 HU is a suspicious feature. Magnetic resonance is recommended to evaluate.
7“Flash-filling” feature: uniform hyperenhancement relative to hepatic parenchyma on arterial phase (including late arterial/early portal venous phase) postcontrast imaging. If additional postcontrast phases are available to characterize the lesion as benign (eg, hemangioma) or suspicious (eg, hepatocellular carcinoma) the lesion should be placed in one of those respective categories and not here.
8Incidental hepatic lesions that are > 1.5 cm and do not have benign features should undergo prompt MRI. Direct biopsy (without MRI) may be appropriate in some scenarios. Differentiation of FNH from adenoma is important, especially if larger than 3 cm and subcapsular in location; for such patients, MRI with gadoxetate disodium is recommended.
9If biopsy is pursued, core biopsy is preferred over fine needle aspiration.
CT indicates computed tomography; FNH, focal nodular hyperplasia; MRI, magnetic resonance imaging.
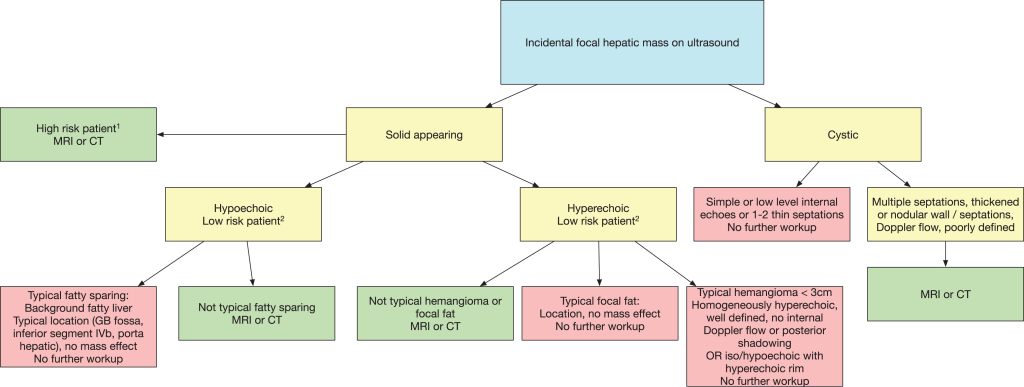
Incidental lesions on US
1Low-risk patient: no known primary malignancy or hepatic risk factors (cirrhosis, hepatitis, alcoholism, nonalcoholic steatohepatitis, sclerosing cholangitis, primary biliary cirrhosis, choledochal cyst, hemochromatosis and other hereditary hepatic conditions, anabolic steroid use, or elevated tumor markers).
2High-risk patient: history of malignancy or hepatic risk factors as previously defined.